COVID-19 from a Public Health Perspective: An Interview with Dr. Timothy Evans
In tandem with my previous article about the impact of COVID-19 on exacerbating inequalities in global health, I looked to the expertise of Dr. Timothy Evans to provide insight on the implications of the pandemic both in Canada and abroad. Dr. Evans is the Director and Associate Dean of the School of Population and Global Health at McGill University. His expansive career has been devoted to promoting health equity around the globe, and he has held several high-profile public health positions, such as Assistant Director General of the World Health Organization and Senior Director of the Health, Nutrition, and Population (HNP) Global Practice at the World Bank Group.
Dr. Evans is the Executive Director of the COVID-19 Immunity Task Force launched by the Government of Canada. The Task Force’s mandate is to implement widespread population-based studies across Canada to estimate the prevalence of SARS-COV-2 immunity and collect information that will influence the ways in which Canada continually manages the COVID-19 epidemic.
This interview took place on July 10, 2020. It has been transcribed and edited for length and clarity.
Alua Kulenova: My first question is about the specific social determinants of health care, how these disparities exist, and how COVID-19 will exacerbate them.
Dr. Timothy Evans: There’s a risk to illness and disease and infection everywhere, which is people with less means and less resources are often disproportionately at greater risk of illness and […] of not being able to access the care they need, or the care that could be available. A British academic, Julian Tudor Hart, wrote about [those things] in 1971 in The Lancet, in an article called “The Inverse Care Law.” It was his observation after 25 years at the NHS in Britain that poorer populations with greater health needs were not getting as much care as better-off populations with less health needs, even in a setting with a universal health care system. This is to say that this gradient, or these gradients, are part of systemic forces of exclusion. We’ve seen a lot of issues related to systemic racism coming into the media. Race, colour of skin, and all sorts of other factors are these fault lines around which you see stratification within and across countries.
In the context of COVID, we shouldn’t be too surprised to see similar patterns emerging. Even though, at one level one would think that biologically, everybody’s [lack of exposure] to this virus means we would be equally susceptible, we find out quickly that actually, if you have a pre-existing condition or you’re immunocompromised, that it does make a difference in terms of mortality. What we’re also finding is that risk of infection and risk of adverse consequences of infection are following racial, ethnic, economic groupings, with the poor and less included segments of populations suffering more.
That’s the harsh reality of this epidemic, not unlike all sorts of other things like HIV, tuberculosis, and malaria. I think the really important thing in this context is to acknowledge it, and then think about how the response both in preparedness and managing the outbreak needs to be much more sensitive to those specific contexts that were risk clusters disproportionately. Just to translate that, in Montréal — which has been one of the epicentres as you know — well-off neighbourhoods like Westmount and Outremont have not seen a lot of cases. But if you move to North Montréal or Côte-Des-Neiges, which are much more ethnically diverse and poor, you see a much, much higher concentration of clustering infections. Yet the testing systems and response systems have assumed a much more equally distributed risk. So the design of our systems needs to be much more responsive to those disproportionate risks. Now, given that we are on the tail-end of phase one and we’ve seen the pattern, we really have an opportunity to re-gear and make sure that we are much more proactive with respect to those higher risk communities.
AK: My second question concerns the global and equal distribution of a vaccine.
Dr. Evans: On vaccines, I think it’s great that the world is mobilizing on developing vaccines and developing them quickly. There are a number of vaccines that are in phase three clinical trials, which is the phase that lets us know whether or not these things are going to have an impact on protecting the population from infection. I’ve been involved with vaccines for a long time, and it always takes us a little longer than we expect. So I think we have to be cautious of feeling like the vaccine is going to be here in December or January.
However, [even] with the prospect of a vaccine, there’s no reason not to be prepared. It is very difficult to roll out anything to the entire population anywhere. My guess is that we’re probably going to have to be faced with some tough decisions on who gets vaccinated first. That doesn’t mean that everybody’s not going to get vaccinated, but there’s going to have to be some criteria that would allow vaccines to move to places and populations where risk is greater. This comes back to your first question — that it shouldn’t be based on your ability to pay, as it might be in the United States. It really needs to be looking at where the benefits of the vaccine are going to be greatest in the first instance. I think we need to work on those and justify [our priorities].
AK: Is it really the case that a vaccine could serve as sort of a social reset in that everything would go back to normal immediately?
Dr. Evans: I think, you know, technologies can be very helpful in changing how we manage things. If we think about HIV, the advent of antiretroviral therapy, the triple therapy, made a huge difference and transformed how we think [about] and deal with the disease. It didn’t take away from the importance of being conscious and cautious with respect to sexually transmitted infections, for example, or for screening blood to make sure you weren’t transmitting infection, so I don’t think it means that you all of a sudden disregard a lot of the important behavioural modifications.
However, it could make a difference. It’s not only a vaccine — we could have a very good treatment and great drugs that make it much less likely that people [get hospitalized] or, if they do go to the hospital, that this is a death sentence. But my sense is that it’s a mistake to put all your eggs in those baskets. It’s very important to ramp efforts up and we’re seeing tremendous mobilization. That makes me more optimistic that we’ll have a technological breakthrough. But that has to be done with some sort of conservative assumption that this will take much longer than we expect. Therefore you have to really invest in our bread and butter of public health, [which is] recognizing that every individual is a public health agent, and encouraging those good behaviours, which we know make a difference.

AK: So I want to use that as a vantage point to segue into Canada’s COVID response and your work with the Task Force. I was wondering, for the purposes of this publication, if you could translate the concept of serological prevalence of antibodies into layman’s terms; share what we know about immunity so far; and discuss what the Task Force has been aiming to do with that information.
Dr. Evans: Antibody testing really just gives you a sense of whether the body, after being exposed to the virus, has mounted an immune response that can be measured by circulating antibodies in the blood. So these tests are designed to detect those antibodies and they give you an indication that a person has been impacted. That’s incredibly important in the context of this virus.
What we’ve found, in a very humbling way, is that a lot of infectiousness of this virus is amongst individuals who are not symptomatic. As many as 40 per cent of people can be infected and never experience any symptoms, at least by their own self-report. In that case, having another test, which shows that you have had an infection, even if you are asymptomatic, is really important. Antibody testing allows us to see the bigger picture of infection taking place in this epidemic that we don’t get when we’re just testing people with symptoms. Seeing the base of the iceberg is very important because it allows us to get a more accurate measure of fatality. Widespread infection rates give us a sense that this virus perhaps is not as lethal as people might think it is. It also gives us an understanding, looking at the distribution of infection, of how the infection is clustering or not in various settings.
From the infection perspective, the antibodies are helpful in understanding whether or not they will provide protection from reinfection and then, very importantly, how long that protection might last. So those are two really, really important questions. We need to be following people out over time who have been infected to see if they become reinfected, or if they do become reinfected, is a second infection much less severe because they have some immune memory, or does this immunity disappear after three months? If immune response doesn’t last long, you may need regular boosters. The immune understanding of the interaction is going to be very important to understanding how to design and apply vaccines.
Those are the two primary questions that are driving the Task Force. It was set up to get information on those questions from across the country. We’re developing the picture of infection from babies to elderly people, across all of our geographies. In addition, we’re looking at high risk occupational groups. We’re also looking at special communities of risk which are defined by ethnic criteria or Indigenous communities, but also geographically and special populations like homeless or incarcerated populations. We’ll be following populations over time to gain insights on these immunity questions. We have a two year mandate, and we think by collecting that information, we’ll be in a position to help inform discussions related to the opening up the economy, development and application of vaccines should they be developed, and also how antibody testing could be used alongside [swab] testing in a complimentary way to inform public health surveillance.
AK: As someone actively working in the fight against COVID as a public health professional, can you speak to the pervasiveness of misinformation about the virus and its potential consequences?
Dr. Evans: The most important lesson in which we learn from COVID is humility, because we constantly had to rethink our understanding, based on observations that really didn’t fit. That’s very, very humbling for public health professionals, because people look to you to be the experts. But the reality is that this virus has out-guessed us or has out-witted us and in many respects, we’re fools not to acknowledge our errors. I think we’re perhaps more likely to make progress if we admit that we were misguided back in March when we didn’t think masks would be helpful. We have to keep ourselves constantly asking, does our advice, our understanding of where things are, really fit with what we’re seeing? What is the real evidence? As opposed to [relying on] hearsay or conspiracy or things like that, ask for real numbers — and I think that’s sometimes helpful for avoiding getting swept up in misinformation.

AK: The wearing of masks has become somewhat of a divisive issue, particularly in the US. How do you think Canadians have fared with accepting scientific evidence and what is the role that the government has had?
Dr. Evans: I think, on the whole, Canadians are more trusting of science and of government. And I think with good reason. Science is helpful. It sometimes has errors and as I mentioned, our understanding has evolved with respect to masks, but the evolution of thinking and recognition that masks are now valuable is not a failure of science. It’s a strength of asking hard questions and understanding where perhaps understanding was not sufficient earlier on.
I think what’s really critical in managing public trust is, first of all, honesty, and in having integrity with respect to the scientific processes that are being stewarded by our institutions. Secondly is giving institutions their due responsibility to do the work that they’re supposed to do and not cutting them off at the knees. I think when you’re in a crisis, there’s no institution that’s working perfectly. My experience is that anybody in those institutions is working to help them perform and respond to challenging circumstances. What’s more important is to look at how to support those institutions to be more effective in crisis, rather than threatening to remove membership or funding. I think that’s backwards thinking and dangerous. I think the point is [to build stronger institutions] and say that we want our institutions to reflect well on us. Opening up and mitigating the worst effects of a second wave is going to be a function of having our institutions in as good shape as possible and preserving trust with the public so that they understand what these institutions are doing. Understand that they’re trying to improve and have communications from them in such a way that their concerns, as they arise, are addressed on an ongoing basis.
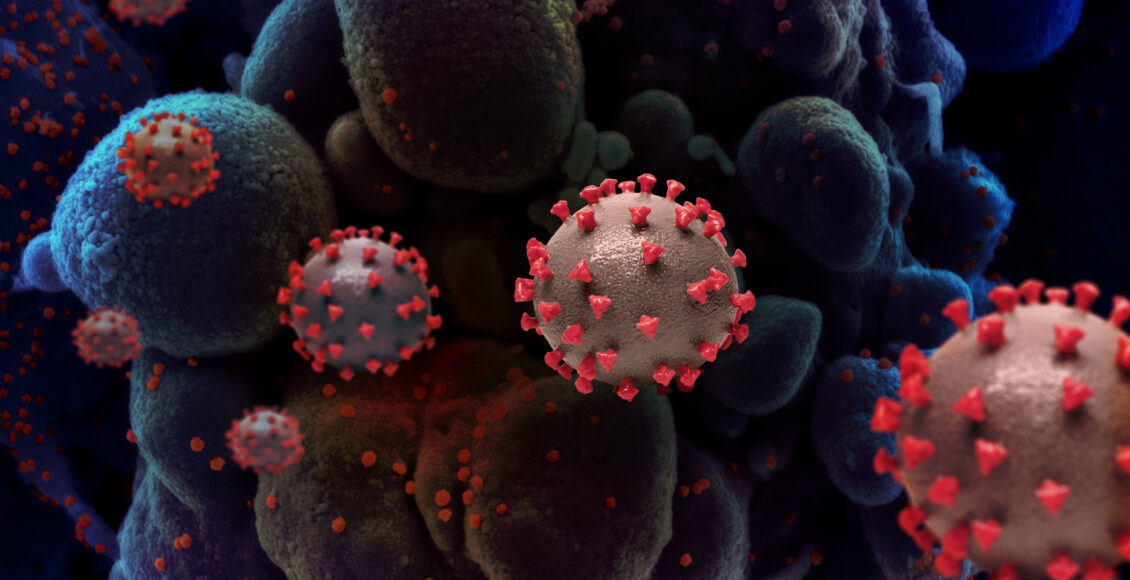
The featured image, “Novel Coronavirus SARS-CoV-2” by NIAID (National Institute of Allergies and Infectious Diseases), is licensed under CC BY 2.0. No changes made.
Edited by Nina Russell
